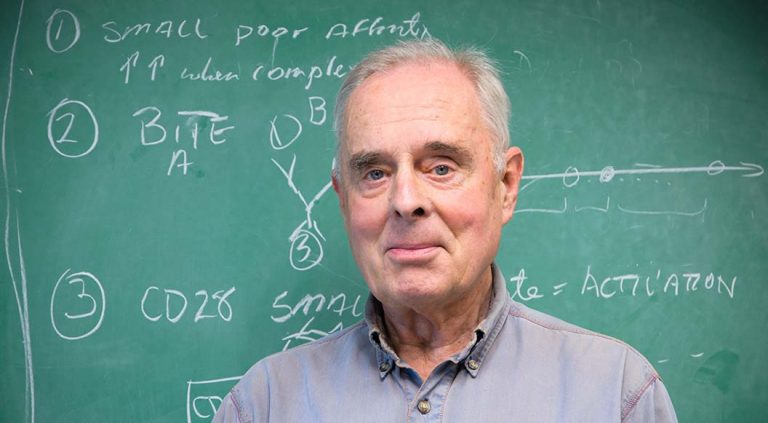
A blackboard hangs in the office of bone marrow transplant pioneer Rainer Storb, MD, in Fred Hutch Cancer Center’s South Lake Union campus in Seattle.
That board is where many of the lifesaving breakthroughs in bone marrow transplantation were mapped out over nearly six decades. First hung in Storb’s office nearly 60 years ago, back when patients receiving the then-highly experimental bone marrow transplant were still irradiated in an underground World War II-era bunker in West Seattle, the board followed Storb to Fred Hutch’s first campus on First Hill and then to South Lake Union.
“We were pretty isolated in the early days,” Storb recalled.
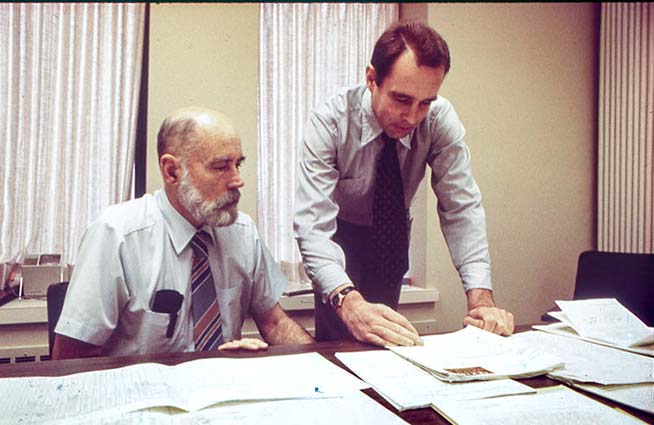
He and the small-but-scrappy bone marrow transplant (BMT) team, led by E. Donnall Thomas, MD, had carved out a couple of floors in a down-at-the heels Public Health Service hospital. Success, and Thomas’ Nobel Prize for BMT, were years in the future. The bunker was six miles away. The hospital’s library was limited, and another six miles (in a different direction) separated the team from their scientific peers at the University of Washington.
But Storb couldn’t remain isolated. Over the ensuing years, he attracted new scientists to the field and built globe-spanning teams to answer the questions that have made the approach easier, safer and available to patients young and old.
In June, to commemorate his 90th birthday and his retirement, world leaders in bone marrow transplant convened at an all-day symposium highlighting Storb’s contributions to science and scientists.
Fred Hutch Executive Vice President Fred Appelbaum, MD, holder of the Metcalfe Family/Frederick Appelbaum Endowed Chair, who worked closely with Storb on bone marrow transplantation, introduced Storb at the symposium and attempted to summarize his ground-breaking work.
“It’s a pretty daunting task,” Appelbaum told the crowd. “That’s 60 years of amazing work. His CV has more pages than almost any of you have papers.”
Storb will receive the 2025 Wallace H. Coulter Award for Lifetime Achievement in Hematology from the American Society of Hematology at ASH’s annual December meeting, and holds the inaugural Milton B. Rubin Family Endowed Chair. To date, he has published 1,615 research papers, a feat made possible by an unbroken stretch of public funding.
This impressive track record is not merely the result of a long tenure in the field, said transplant biologist and long-time Storb collaborator Marco Mielcarek, MD, medical director of Adult Blood and Marrow Transplantation at Fred Hutch.
“Rainer has been incredibly productive with countless important contributions to the field. His cumulative knowledge is the result of his inquisitory nature combined with his tireless and infectious work ethic,” Mielcarek said, estimating that over Storb’s many years of scientific endeavor, his energy allowed him to accumulate about two lifetimes’ worth of transplant experience.
Scientist: collaborator and patient advocate
Storb arrived in Seattle in 1965, on a Fulbright scholarship with several high-profile publications already under his belt. After training as a doctor in Germany, Storb had worked with Marcel Bessis, MD, in Paris to understand the function of various subcellular organelles by using laser beams to damage them after treating cells with various vital dyes.
“It was a very productive time, but I got so far away from the clinic,” Storb recalled.
Hoping to find his way back to patient-centered work, he quizzed visiting scientists about the most cutting-edge clinical research and read up on their recommendations in the library.
“The most interesting name was Don Thomas,” Storb said. So he wrote Thomas a letter, and three weeks later received a reply inviting him to join the fledgling team.
Bone marrow transplantation aims to wipe out blood cancer at its source, the bone marrow, and replace it with healthy, non-cancerous donated marrow cells. These can then regrow all the oxygen-carrying, disease-fighting and wound-healing properties of healthy blood-cell system. On its face, the idea made sense. But at the time, scientists didn’t understand how the strategies our immune system uses to ward off danger could doom genetically distinct donor cells. Promising results in inbred mice had failed to translate to genetically varied humans.
Few remained who believed it could work. Joining Thomas’ team took deep dedication and a high tolerance for risk. Luckily, Storb’s ambition and energy carried him through the early failures, even as he and the team dedicated nearly every waking hour — weekends not excepted — to their vision.
A much-needed breakthrough occurred in 1967 when Storb had nearly given up hope. He and colleague Bob Epstein, MD, then the only other member of Thomas’ team, showed that pre-transplant tissue-type matching was an essential step to the strategy’s success. After that, the field began picking up momentum and never stopped.
Storb was a key player in many of the advancements that made bone marrow transplantation work, symposium participants said.
“He developed preclinical models which are still the base for current protocols including a safer conditioning regimen that reduced transplant treatment-related mortality. He was a pioneer in the use of immunosuppressive drugs to prevent graft-vs.-host disease or GVHD, he established the protocol for donor selection and tissue matching,” said transplant biologist Eliane Gluckman, MD, PhD. She was trained by Storb in Seattle in 1973 and developed in France one of the first bone marrow transplant units in Europe where she performed the first successful in-human umbilical cord blood transplant in 1988. She was a founding member of the European Group of Bone Marrow Transplantation in 1974.
Storb established preclinical models that allowed scientists to work out the biology and genes behind tissue typing. Working with dogs, the team essentially conducted canine clinical trials, enrolling family pets with cancer in transplant trials that often saved their lives while establishing principles that could be applied to humans as well.
“All of the advances that we made in leukemia and malignant diseases, Rainer was also instrumental in,” Appelbaum said — but initially Storb and Thomas took the work in slightly different directions. Thomas focused on blood cancers, and Storb explored BMT’s potential to treat noncancerous blood disorders.
Storb showed that BMT could cure aplastic anemia, a blood disorder in which a patient’s bone marrow fails to make enough blood cells, and developed a treatment regimen that’s still in use today.
Many of Storb’s colleagues touched on his determination, unflagging curiosity and commitment to understanding results — even those that might first appear to be a mistake.
“One of the biggest embedded inspirations in what Rainer has done, and the Hutch has done, is to not let any patient go unstudied,” said Storb symposium speaker Leslie Kean, MD, PhD, who directs the Pediatric Stem Cell Transplant Program at Dana-Farber/Boston Children’s Cancer and Blood Disorders Center.
Mini-transplantation, one of Storb’s proudest achievements, uses a gentler regimen (known as non-myeloablative conditioning) and has enabled older blood cancer patients to receive bone marrow transplants. But it grew out of a mistake.
In a preclinical model of BMT, some of the animals had been mistakenly given a lower dose of radiation than normal — but the donor stem cells still engrafted in a few. Storb wanted to explore the concept, but initially couldn’t get NIH funding for his off-the-wall idea. Seed money from the grateful father of a patient got him started.
Patients receiving a standard BMT undergo a grueling pre-transplant regimen and spend weeks in the hospital. The first patient who received a mini-transplant, for chronic lymphocytic leukemia, “Didn’t even see a hospital from the inside,” Storb said. “He was totally outpatient, he didn’t even lose his hair.”
At the time, “the old age in transplant was 55, which was the upper limit of what we were transplanting at the time — until this disruptive paper came out,” said Stanford University transplant researcher Judith Shizuru, PhD, who joined the network of researchers, assembled by Storb, to move the concept of non-myeloablative conditioning regimens forward.
“Someone else might [look at that experiment and] say, ‘Oh that’s not quite what I wanted,’ and ignore that interesting finding,” said Fred Hutch bone marrow transplant researcher Brenda Sandmaier, MD, who has worked closely with Storb since she joined Fred Hutch in the mid-1980s. Sandmaier is deputy director of Fred Hutch’s Translational Science and Therapeutics Division.
“But instead he said, ‘This is very interesting. I want to look at this, I want to investigate it,’” Sandmaier said. “To me, it’s very illuminating on how you do science. You have a hypothesis and you think you’re answering the question — but if you get some strange result, you don’t ignore it.”
Storb’s interest in mini-transplantation was also inspired by work he had published in 1979, the first large-scale study detailing the ability of donated cells to stave off leukemia relapse. Mini transplants rely on donated immune cells, rather than harsh drugs and radiation, to kill off cancer cells.
In the late 1970s, BMT researchers were more concerned with controlling the often-deadly graft-vs.-host disease, or GVHD, than capitalizing on graft-vs.-leukemia, or GVL. But as transplant improved and technologies advanced, the finding helped inspire not only the mini-transplant, but today’s cellular cancer immunotherapies.
The early days, however, were very low-tech.
“We did a lot of stuff with our own hands and that’s I guess what helped us with translating [the preclinical work to patients],” Storb said. He and colleague Bob Epstein spent time treating transplant patients “and that helped us in understanding where things were still going wrong, and we took that back to the lab. Being a physician-scientist was critical.”
Symposium speakers noted the consistent quality of Storb’s output. Just last year, Storb and collaborators led by Fred Hutch’s Masumi Ueda Oshida, MD, MA, tackled a long-standing question about whether mutations in donor cells are likely to drive accelerated cell growth and eventually leukemia. They found that donated cells don’t acquire mutations at a higher rate in recipients than donors, and even cells from the youngest donor in the study (age 12) harbor genetic changes associated with cancer. But these changes don’t cause a higher risk of disease later, according to the work, published in Science Translational Medicine.
Mentor: warm and welcoming
As long as he has been a scientist, Storb has also been a trusted resource for his colleagues.
“He’s persuasive, persistent — perhaps almost to a fault,” Mielcarek said, who credits Storb and his late wife, Beverly Torok-Storb, PhD, as his “scientific parents.” Storb made sure mentees published their work, even the negative results, to ensure that every experiment or clinical trial enriched the field, Mielcarek said.
“He’s very proud of having had uninterrupted NIH [National Institutes of Health] funding from his early days,” Mielcarek said. “It’s taxpayer dollars, so he feels a sense of responsibility, that the public deserves to hear what came out of the research.”
Storb’s famous open-door policy applied to everyone, whether a formally acknowledged mentee or not. Storb’s energy and passion helped buoy other’s careers as well, and many scientists who built transplant centers around the world trained under Storb, Mielcarek said.
At the symposium, Sandmaier presented a map, created by Fred Hutch technical editor and longtime Storb collaborator Helen Crawford, showing Storb’s global reach: 160 trainees from 27 countries and five continents.
Kean recalled visiting Storb from her home base at Emory University and consulting with him regarding setting up a new model of bone marrow transplantation.
“The wisdom you imparted to me was really transformational,” she told him. You just can’t understand all of the essential details from reading a paper when you’re trying to create a new model; you have to get the direct experience from someone who’s been in the trenches.”
And Storb’s advice integrated his experience in the trenches and the bird’s-eye view of the field he’d gained through decades of experience.
Sandmaier remembered the support he offered when she was wavering on whether alpha-emitter radioimmunotherapy, a more-targeted approach to cancer radiation that she was developing in preclinical models, was ready to bring to patients. He told her it was.
“Because if you’re developing something to go into patients, to make things better for patients, you have to make that leap,” Sandmaier said. “He had broad experience of doing that, not once but many times.”
Sandmaier, Mielcarek and many symposium attendees remembered the warm and welcoming community Storb and Torok-Storb created, at Fred Hutch and beyond. They often invited young researchers to dinners at their home and on the outdoor activities they both loved.
“He loved the mountains. … He loved to take his lab and everybody else who would be willing to go on some hiking trip,” Sandmaier said. “He realized not everybody was as fit as him. So then he’d be thoughtful: OK, what’s a hike the whole group could do? He was just as competitive as he was in the science, but he also wanted to share that with everybody, his great love of sports.”
Storb won’t be retiring to nap in the sun. He’ll be focusing on his other interests, including the sculling that he took up in his late 40s. Storb went on to compete in (and win) many races and is well-known for having rowed himself to work through South Lake Union for many years. Maybe he’ll find the time to write down his incredible life.
“He’s just a very broadly interested person and educated in a different way,” said Sandmaier, who noted that Storb could also speak about the architecture of various European cities and the migration patterns that shaped Europe and countries elsewhere. “His mind is just so active; it’s not just science.”
She got her own shout-out at Storb’s symposium.
“Great mentors create great mentors,” said Kean, who noted that Sandmaier had mentored her throughout her career: “I think this says a lot, the legacy of mentor to mentor, so thank you.”
As Storb steps away from his projects, an era in transplant biology comes to an end.
“Rainer, you’ve been a constant and positive force who has led this bone marrow transplant community to always strive to do better for the people that we treat and those that we hope to treat,” Shizuru said. “I can’t help but think that these values, plus your incredible passion for what you do, is really the key to your eternal youth. I realized this morning that you’re not a boomer, but regardless, you rock.”